 A pigmented nail lesion is a concern that comes up more often than you would think, and most people don’t know what to do about it. The potential of melanoma can be scary, and many people aren’t comfortable dealing with nails. However, I typically see around two patients a month with pigmented nail lesions who have received referrals from dermatology offices.
A pigmented nail lesion is a concern that comes up more often than you would think, and most people don’t know what to do about it. The potential of melanoma can be scary, and many people aren’t comfortable dealing with nails. However, I typically see around two patients a month with pigmented nail lesions who have received referrals from dermatology offices.
Understanding Melanoma
It is estimated that the number of melanoma cases diagnosed in the US will increase by almost 6% to over 200,000 cases. The reason for the increase is not entirely clear. A vast majority of skin cancers (est 90%) are due to UV radiation from sun exposure.
The increased incidence of skin cancers may be due to longer lifespans, climate change, and the prevalence of indoor tanning beds. One area related to the diagnosis and treatment of skin cancer is the evaluation and management of pigmented lesions of the nail bed and surrounding area. This is a topic that often confuses patients, primary care physicians, and specialists alike.
Are Pigmented Nail Lesions Cancerous?
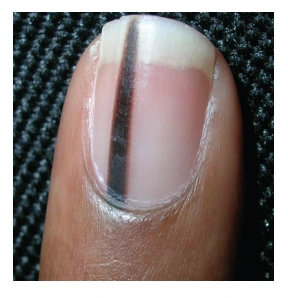
The vast majority of pigmented nail lesions are benign. Longitudinal pigmented streaks are known as longitudinal melanonychia or melanonychia striata. The differential diagnosis of pigmented nail lesions includes fungal infections, viral wart, subungual hematoma (blood collection), medication-induced pigment (chemotherapy), ethnic-type pigmentation, benign nevus, squamous cell carcinoma,
and melanoma.
The clinical examination always begins with a thorough history including the duration of the pigmented lesion, any changes over time, history of trauma, and family history of melanoma.
There are several clinical factors to keep in mind that help differentiate benign from potentially malignant nail pigmentation:
- Age – 50–70
- Ethnicity – Acral lentiginous melanoma is more common in those of Asian, African-American, and Native American descent.
- Lesion width – >3mm concerning for malignancy
- Coloration – Gray/tan vs. darker brown/black
- Borders – Sharp distinct borders usually suggest a benign lesion.
- Change – Rapid increase in size or change in morphology
- Digit involved – The thumb/great toe is most common. Typically a single digit =malignancy, and multiple digits = benign.
- Hutchinson’s sign – Pigmentation on the nail fold is highly suspicious for melanoma.
- Family history of melanoma
Treating Pigmented Nail Lesions
Benign appearing pigmented nail lesions can be safely observed. This is the case with most nail pigment. Most sources recommend re-evaluation every 3 months initially to evaluate for changes. Serial photographs can help track any changes that may occur. Patients can be treated for a fungal infection with oral or topical anti-fungal to see if the nail coloration or nail dystrophy resolves. Pigmented lesions that present with any malignant features should be biopsied. I will offer a biopsy to patients with equivocal lesions for peace of mind, and I have not found any that regret receiving a negative biopsy result.
Proper biopsy technique involves a full thickness excision of nailbed tissue down to bone involving any visible pigment. I perform these under local anesthesia and tourniquet control as an office procedure. The nail is elevated off the nailbed and relaxing incisions are made in the corners of the nail fold. The nail fold with the nail attached are reflected back proximally. This gives a complete view of the nailbed and germinal matrix as the pigmented lesions often originate in the germinal matrix under the nail fold. The tissue is excised with a scalpel or punch. A scalpel is used to undermine the nailbed tissue and close the biopsy site without tension using absorbable sutures. This minimizes any post-operative nail deformity. The nail is then replaced and sutured down. Patients are back to full activities in a week with minimal long-term issues.
Any suspicious pigmented nail lesions should be evaluated by a dermatologist or hand surgeon to determine the need for a biopsy and further treatment.
If you have questions or would like to schedule an appointment, contact the hand surgeons at The Institute for Hand Surgery at New York Plastic Surgical Group.
Previous Post Next Post

